Psychiatric History Template
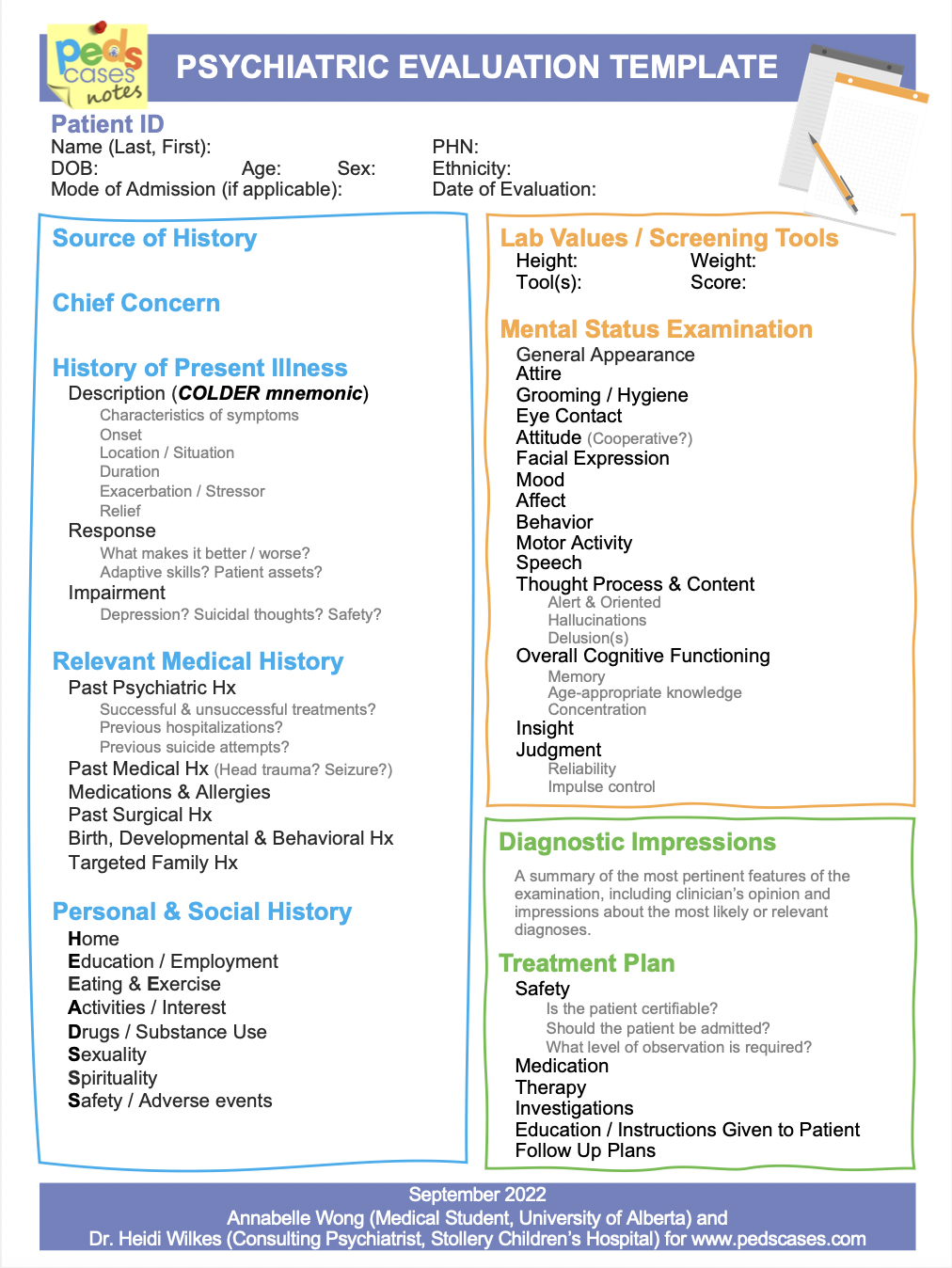
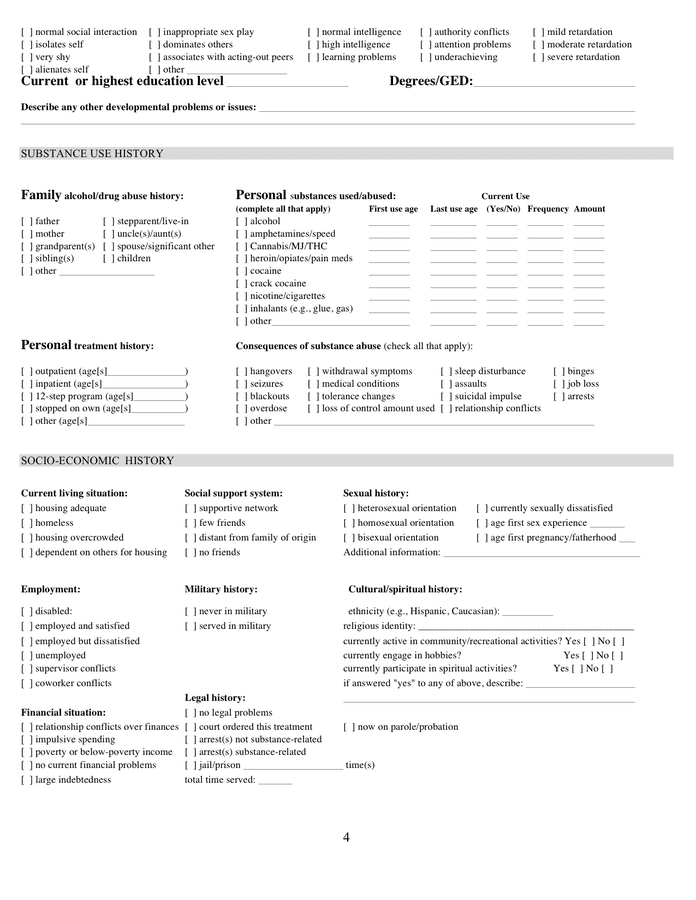
Psychiatric History Template - An initial psychiatric evaluation note with all components of the initial evaluation including history of present illness, past medical history, social history, mental status examination, diagnostic. chief complaint (this can be in the patient’s own words or a. History of present illness (hpi) (1) develops illness narrative: Are you always anxious or does it happen at certain. Each template can be customized to fit individual needs, and. A practical guide to the clinical interview 3. Templates can be especially helpful for routine. you’ll want to have a template that includes the following sections: Psychiatric hx previous psychiatric hx/counseling/suicide attempts/violence: What should you include in your initial psychiatric evaluation? you’ll want to have a template that includes the following sections: This document outlines a psychiatric history taking format that includes: An initial psychiatric evaluation note with all components of the initial evaluation including history of present illness, past medical history, social history, mental status examination, diagnostic. Download or preview 4 pages of pdf version of medical psychiatric history form (doc: Templates can be especially helpful for routine. chief complaint (this can be in the patient’s own words or a. What should you include in your initial psychiatric evaluation? Are you always anxious or does it happen at certain. A guide for medical students on how to write a comprehensive and structured psychiatric case history. 153.3 kb ) for free. A practical guide to the clinical interview 3. 153.3 kb ) for free. Identifying information about the patient and details of their chief complaint and history of present illness. Templates can be especially helpful for routine. Are you always anxious or does it happen at certain. Includes general instructions, sections, examples and tips for presenting a patient's. A practical guide to the clinical interview 3. Each template can be customized to fit individual needs, and. (cogent story with clear chronology, not a list of symptoms), and (2) includes specific details of symptoms, and the impact of these. History of present illness (hpi) (1) develops illness narrative: you’ll want to have a template that includes the following sections: Includes general instructions, sections, examples and tips for presenting a patient's. Osmind simplifies the process of writing psychiatry progress notes with over 60 templates tailored to for mental health clinicians. What should you include in your initial psychiatric evaluation? Download or preview 4 pages of pdf version of. This document outlines a psychiatric history taking format that includes: chief complaint (this can be in the patient’s own words or a. Psychiatric hx previous psychiatric hx/counseling/suicide attempts/violence: Past psychiatric history 13 ask the patient about their past psychiatric history 14 establish past psychiatric diagnoses, treatments and past contact with mental health you’ll want to have a template. Bipolar disorder anger alcohol abuse chief complaint (this can be in the patient’s own words or a. Includes general instructions, sections, examples and tips for presenting a patient's. (cogent story with clear chronology, not a list of symptoms), and (2) includes specific details of symptoms, and the impact of these. Psychiatric hx previous psychiatric hx/counseling/suicide attempts/violence: Includes general instructions, sections, examples and tips for presenting a patient's. This document outlines a psychiatric history taking format that includes: Psychiatric hx previous psychiatric hx/counseling/suicide attempts/violence: Each template can be customized to fit individual needs, and. you’ll want to have a template that includes the following sections: This document outlines a psychiatric history taking format that includes: What should you include in your initial psychiatric evaluation? you’ll want to have a template that includes the following sections: A practical guide to the clinical interview 3. Past psychiatric history 13 ask the patient about their past psychiatric history 14 establish past psychiatric diagnoses, treatments and past contact. History of present illness (hpi) (1) develops illness narrative: Osmind simplifies the process of writing psychiatry progress notes with over 60 templates tailored to for mental health clinicians. An initial psychiatric evaluation note with all components of the initial evaluation including history of present illness, past medical history, social history, mental status examination, diagnostic. Each template can be customized to. Are you always anxious or does it happen at certain. An initial psychiatric evaluation note with all components of the initial evaluation including history of present illness, past medical history, social history, mental status examination, diagnostic. This document outlines a psychiatric history taking format that includes: Hasnyone a in your family been diagnosed with or treated for any of the. (cogent story with clear chronology, not a list of symptoms), and (2) includes specific details of symptoms, and the impact of these. Are you always anxious or does it happen at certain. 153.3 kb ) for free. Identifying information about the patient and details of their chief complaint and history of present illness. Each template can be customized to fit. Includes general instructions, sections, examples and tips for presenting a patient's. A guide for medical students on how to write a comprehensive and structured psychiatric case history. A practical guide to the clinical interview 3. History of present illness (hpi) (1) develops illness narrative: Bipolar disorder anger alcohol abuse What should you include in your initial psychiatric evaluation? Download or preview 4 pages of pdf version of medical psychiatric history form (doc: Past psychiatric history 13 ask the patient about their past psychiatric history 14 establish past psychiatric diagnoses, treatments and past contact with mental health An initial psychiatric evaluation note with all components of the initial evaluation including history of present illness, past medical history, social history, mental status examination, diagnostic. Hasnyone a in your family been diagnosed with or treated for any of the following (circle): Each template can be customized to fit individual needs, and. Are you always anxious or does it happen at certain. Identifying information about the patient and details of their chief complaint and history of present illness. Psychiatric hx previous psychiatric hx/counseling/suicide attempts/violence: chief complaint (this can be in the patient’s own words or a. (cogent story with clear chronology, not a list of symptoms), and (2) includes specific details of symptoms, and the impact of these.Psychiatric Evaluation Template PedsCases
Psychiatric History Template
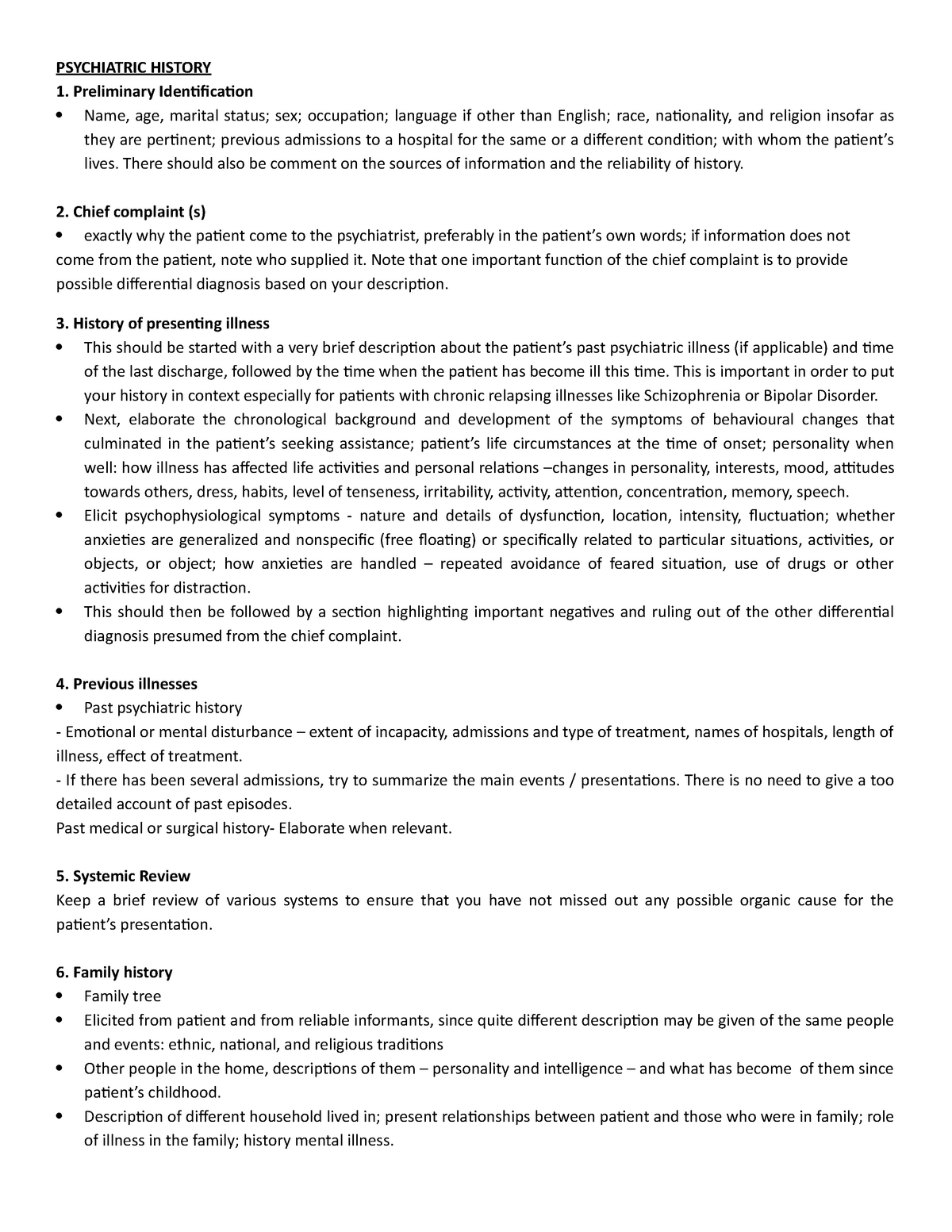
Psych History Template PSYCHIATRIC HISTORY Preliminary Identification
Psychiatric Initial Evaluation Template Printable Templates Free
Full Psychiatric Evaluation Template
Psychiatry Progress Note Template & Example Free PDF Download
Psychiatric Intake Template
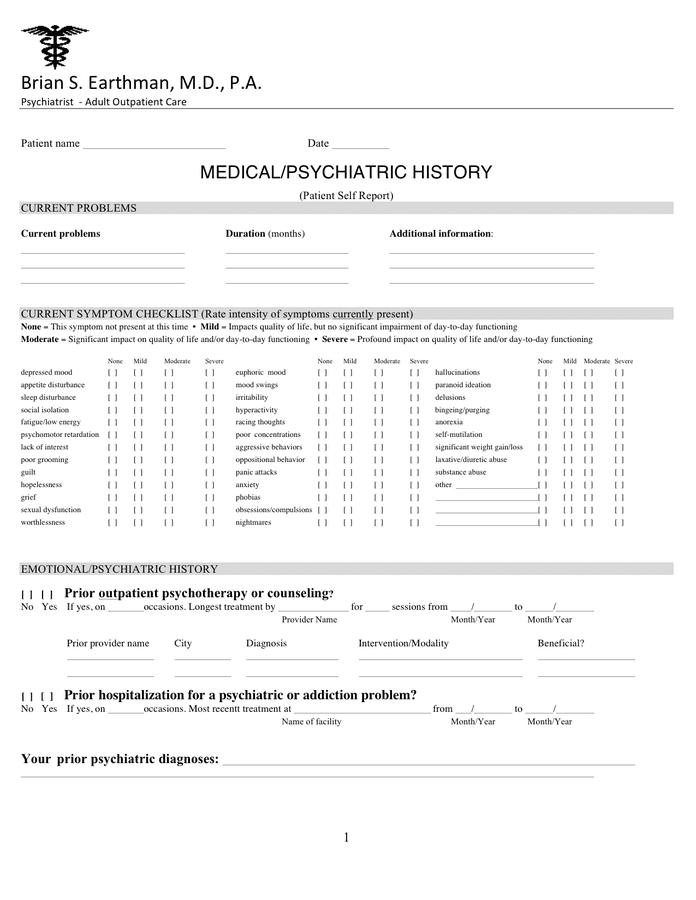
Psychiatric Intake Form / Evaluation PDF Template
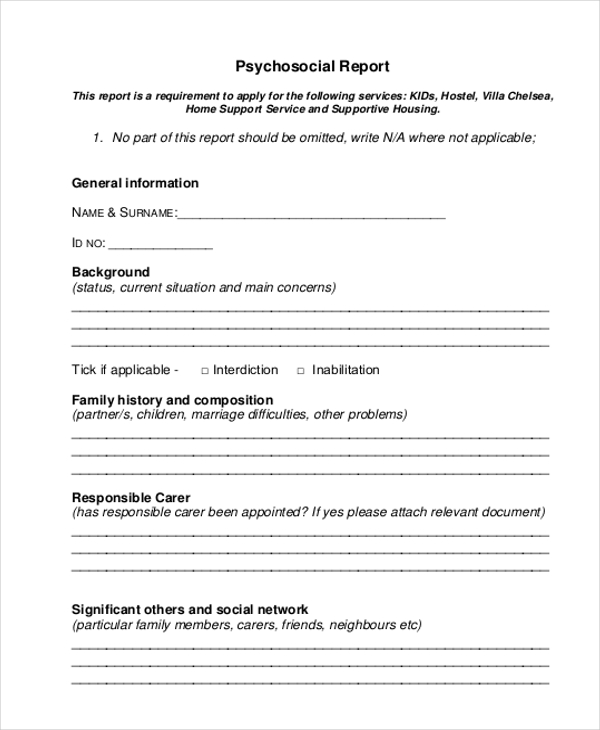
FREE 11+ Psychosocial Assessment Form Samples, PDF, MS Word, Google Docs
Psychiatric History Template
153.3 Kb ) For Free.
Osmind Simplifies The Process Of Writing Psychiatry Progress Notes With Over 60 Templates Tailored To For Mental Health Clinicians.
Templates Can Be Especially Helpful For Routine.
You’ll Want To Have A Template That Includes The Following Sections:
Related Post: