Pt Soap Note Template
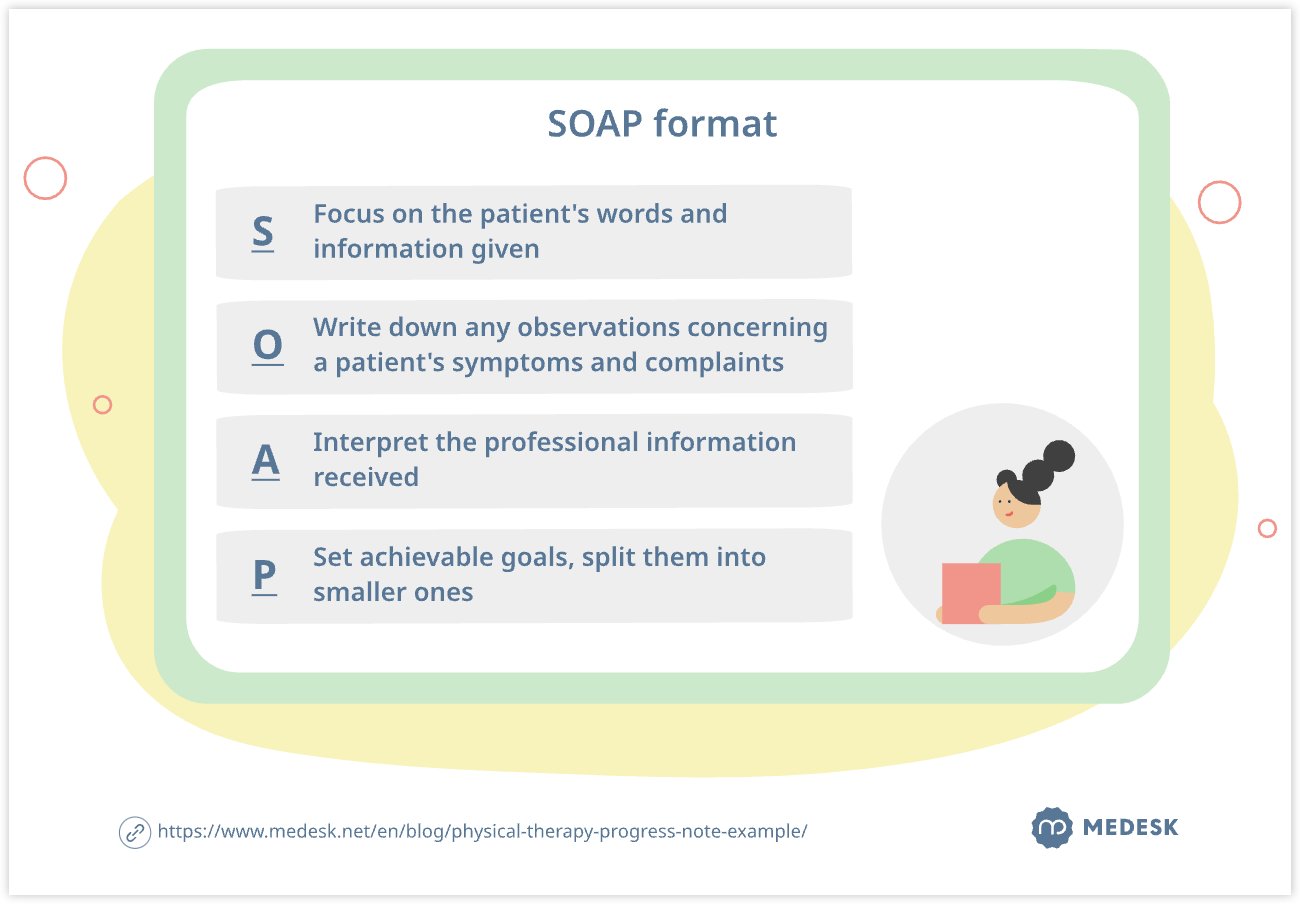
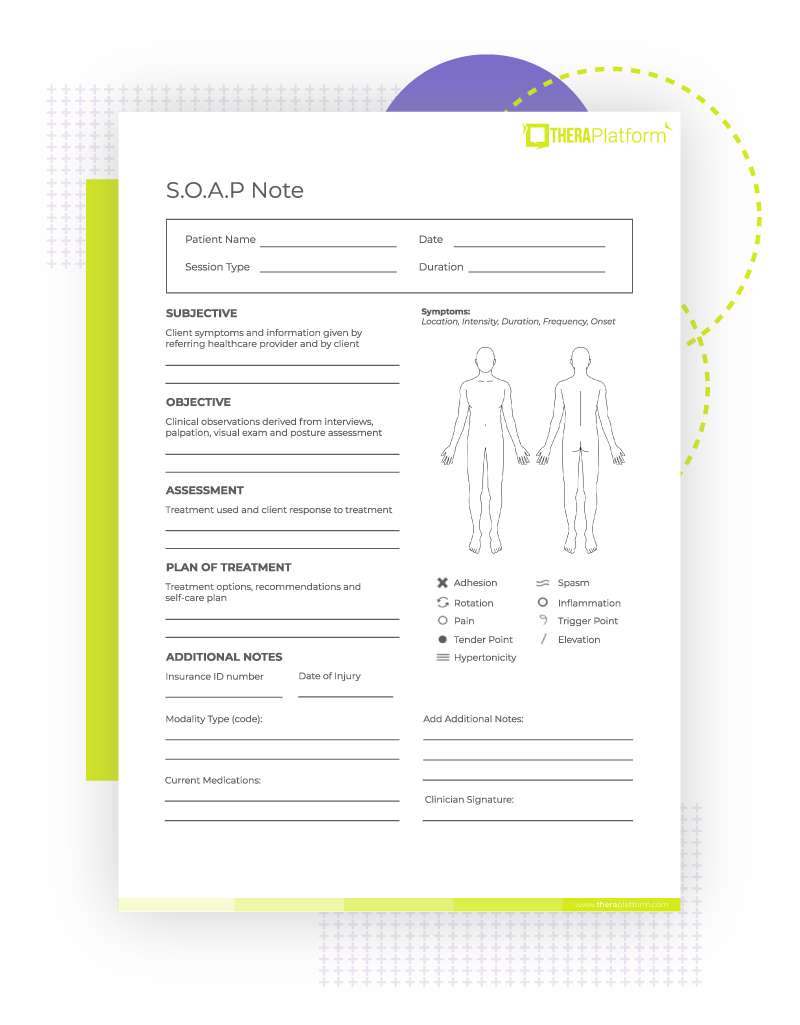
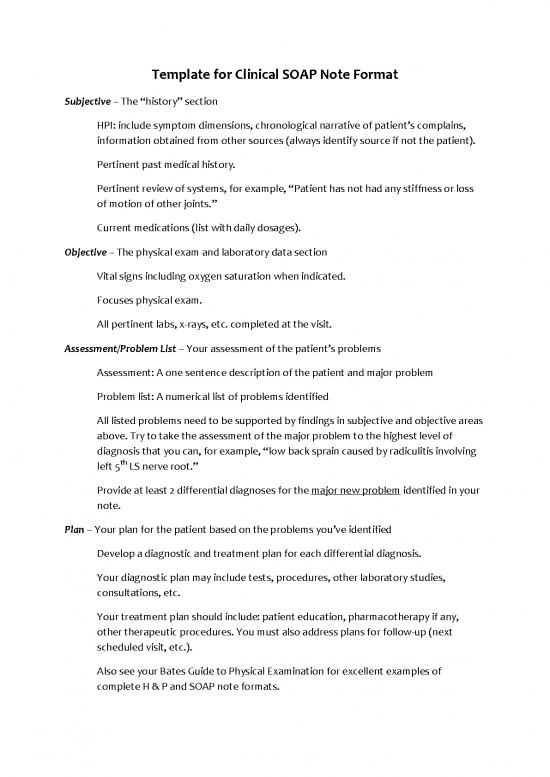
Pt Soap Note Template - Our free, downloadable physical therapy soap note template includes examples of each section including subjective, objective, assessment, and plan. Using a standardized soap note template enhances healthcare service quality by ensuring efficient documentation, organization, and compliance. This guide provides detailed instructions for each section of a soap note, helping you understand. Soap notes are written documentation made during the course of treatment of a patient. A soap note template comes in a very structured format though it is only one of the numerous formats. The patient reports sudden onset of lower back pain after lifting a heavy box two days ago. Wondering how to write soap notes? We will break the process of how to write a soap note into digestible sections in this piece and explain how pts should go about doing so. The soap note isn’t just a record; The patient’s personal report (subjective), what is observed and measured (objective), the. Soap notes are written documentation made during the course of treatment of a patient. This guide provides detailed instructions for each section of a soap note, helping you understand. pt assessment example with soap note when creating physical therapy assessment notes, utilizing a structured template can enhance clarity and consistency. Soap notes are a standardized form of note taking that can serve as evidence of patient contact and effectively communicate important information to the entire care team. Physical therapy soap notes are a specific format of progress notes that physical therapists can use to organize their documentation in a consistent and coherent way. They are commonly used by mental health professionals such as. Using a standardized soap note template enhances healthcare service quality by ensuring efficient documentation, organization, and compliance. We will break the process of how to write a soap note into digestible sections in this piece and explain how pts should go about doing so. Before we discuss how to construct them individually, let’s look at how they fit into the big picture of a completed soap. It’s a testament to the clinician’s. Using a standardized soap note template enhances healthcare service quality by ensuring efficient documentation, organization, and compliance. The patient reports sudden onset of lower back pain after lifting a heavy box two days ago. The soap note isn’t just a record; Our free, downloadable physical therapy soap note template includes examples of each section including subjective, objective, assessment, and plan.. A soap note template is a structured method for documenting patient encounters, commonly used in medical settings. Wondering how to write soap notes? Dap notes are progress notes used to document therapy sessions and track the progress of a treatment process. Download our free soap note template. Using a pt soap note. The soap format can be one of the most effective ways for clinicians to document and objectively assess,. Physical therapy soap notes present a template for capturing (most) of the essential components of a daily visit and when used correctly, will give you the confidence to master your daily. Using a pt soap note. Here’s a revised—and more detailed—example of. What is a soap note? The patient’s personal report (subjective), what is observed and measured (objective), the. Download our free soap note template. They are commonly used by mental health professionals such as. Using a pt soap note. Wondering how to write soap notes? A soap note template is a structured method for documenting patient encounters, commonly used in medical settings. Download our free soap note template. It’s a testament to the clinician’s. Our free, downloadable physical therapy soap note template includes examples of each section including subjective, objective, assessment, and plan. The soap format can be one of the most effective ways for clinicians to document and objectively assess,. The soap note isn’t just a record; Wondering how to write soap notes? Download our free soap note template. The patient’s personal report (subjective), what is observed and measured (objective), the. It’s a testament to the clinician’s. Our free, downloadable physical therapy soap note template includes examples of each section including subjective, objective, assessment, and plan. Physical therapy soap notes are a specific format of progress notes that physical therapists can use to organize their documentation in a consistent and coherent way. Soap notes are a standardized form of note taking. The patient reports sudden onset of lower back pain after lifting a heavy box two days ago. The acronym stands for subjective, objective,. Before we discuss how to construct them individually, let’s look at how they fit into the big picture of a completed soap. This guide provides detailed instructions for each section of a soap note, helping you understand.. Download our free soap note template. Physical therapy soap notes present a template for capturing (most) of the essential components of a daily visit and when used correctly, will give you the confidence to master your daily. Soap notes are a standardized form of note taking that can serve as evidence of patient contact and effectively communicate important information to. We will break the process of how to write a soap note into digestible sections in this piece and explain how pts should go about doing so. A soap note template comes in a very structured format though it is only one of the numerous formats. Using a pt soap note. The soap format can be one of the most. The acronym stands for subjective, objective,. Soap notes are a standardized form of note taking that can serve as evidence of patient contact and effectively communicate important information to the entire care team. The patient reports sudden onset of lower back pain after lifting a heavy box two days ago. They are commonly used by mental health professionals such as. pt assessment example with soap note when creating physical therapy assessment notes, utilizing a structured template can enhance clarity and consistency. The patient’s personal report (subjective), what is observed and measured (objective), the. Wondering how to write soap notes? A soap note template is a structured method for documenting patient encounters, commonly used in medical settings. Soap notes are written documentation made during the course of treatment of a patient. Soap notes are essential for effective patient care and documentation in physical therapy. Start with 3 free soap notes. Download our free soap note template. Before we discuss how to construct them individually, let’s look at how they fit into the big picture of a completed soap. Using a standardized soap note template enhances healthcare service quality by ensuring efficient documentation, organization, and compliance. This guide provides detailed instructions for each section of a soap note, helping you understand. Physical therapy soap notes present a template for capturing (most) of the essential components of a daily visit and when used correctly, will give you the confidence to master your daily.Soap Note Template Physical Therapy
10+ Soap Note Template Free Download Word, Excel, PDF Format!!
Physical therapy soap Notes Template Letter Example Template
Physical Therapy SOAP Note Interactive PDF Template
How to Write The Perfect Physical Therapy SOAP Note + Examples and
Physical Therapy Soap Note Pdf 109589 Template Clin Soap Note
Physical Therapy Soap Note Template
SOAP Notes For Physical Therapy Template & Example Free PDF Download
Free Physical Therapy SOAP Note PDF SafetyCulture
Physical Therapy Progress Note Example Save Time During Appointments
Using A Pt Soap Note.
A Soap Note Template Comes In A Very Structured Format Though It Is Only One Of The Numerous Formats.
The Soap Note Isn’t Just A Record;
Dap Notes Are Progress Notes Used To Document Therapy Sessions And Track The Progress Of A Treatment Process.
Related Post:





.png)